I’d like to introduce you to a practical 6-week diagnostic protocol I’ve developed over the years to help me better understand the patient’s bruxism profile or phenotype.
Nociceptive Trigeminal Inhibition Tension Suppression System (NTI-tss)
I have been using the NTI device since 1998. The NTI-tss is an easily customizable, commercially available segmental intraoral device that engages the Trigeminal jaw-opening reflex - a polysynaptic relay involving interneurons, nociceptors and mechanoreceptors in the periodontal ligament. (Fig. 12) Despite providing arguably minimal supportive clinical research evidence[1] the manufacturer managed to gain FDA approval for its use in the treatment of bruxism, TMD, occlusal trauma as well as the prophylactic non-pharmaceutical management of migraine and tension-type headaches.
Fig. 12A Sleep NTI - Usually made on the upper arch.
Fig. 12B Always ensure that the discluding element is perpendicular to the opposing incisor.
Fig. 12C Awake NTI - Usually made on the lower arch as it interferes less with speech. Notice also the cervical abfraction lesions and the bony exostoses related to Awake Bruxism in this patient.
Fig. 12D There must be no posterior tooth contacts in centric and eccentric mandibular excursions.
Nevertheless, it has been my clinical observation that those who exhibited clenching (tonic NREM SB) versus grinding (phasic NREM SB) during sleep responded better to the NTI rather than traditional Michigan-type occlusal splint design. It was as if the posterior occlusal contact opportunities presented by conventional nightguards allowed clenchers to clench even more and many awoke with worse masticatory muscle aches!
There is some support from the scientific literature for the above. We already know that awake jaw elevator muscle activity was significantly decreased when subjects voluntarily clenched on an anterior bite stop versus when the posterior teeth were in maximum intercuspation [2]. A strong and lasting inhibitory effect on EMG activity in masseter muscles during sleep was also documented when subjects wore the NTI but not the conventional full occlusal coverage splint [3]. That chronic clenching was a common factor in the triggering of migraine and tension-type headaches was supported by findings from an open labelled randomized controlled trial that 82% of NTI users experienced a 77% average reduction in migraine events [4].
Thus, besides awake clenching and NREM tonic SB, I also frequently indicate the NTI for female migraineurs who have to be taken off teratogenic prophylactic medication once they want to start a family.
The 6-week NTI trial
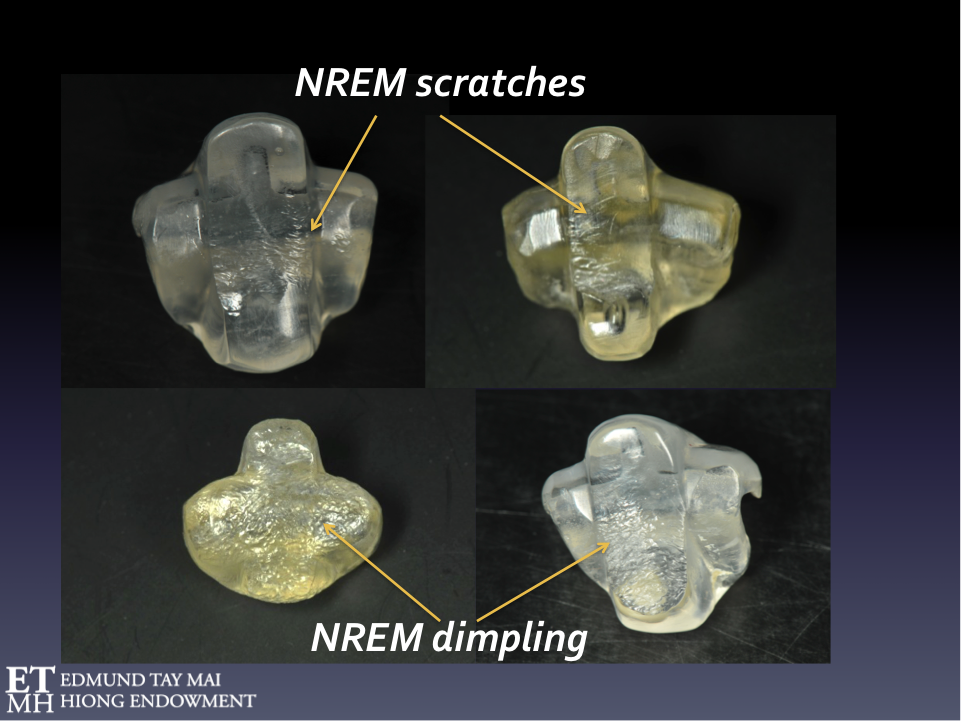
Whilst most patients referred for the management of sleep bruxism showed typical scratches and 'dimpling' on the NTI (Fig.13a), I began to notice a distinct wear pattern emerging in a small subgroup. About 25% of patients referred to me specifically for full-mouth prosthodontic rehabilitation returned after 4-6 weeks with a huge groove on the discluding platform of the sleep NTI and some even complained of TM joint pain on waking. (Fig.13b)
Fig. 13A Typical NREM SB wear patterns on the sleep NTI
Fig. 13B Characteristic REM SB wear pattern on the sleep NTI
Then I had my EUREKA moment! The Trigeminal jaw-opening reflex, like all other protective reflexes, is attenuated during REM sleep. Therefore, the NTI would be ineffective in reducing elevator muscle activity if the patient's bruxism occurs during the REM phase of sleep. This unbridled parasomniac activity over a period produces a recognizable wear pattern on the polycarbonate discluding element of the NTI device which I termed a ‘Divot’ (pardon the golf terminology). When I sent these patients for a full PSG investigation, I discovered that every single one of them presenting with this pathognomonic divot exhibited REM sleep bruxism!
Thus after many such confirmatory PSG exercises, the occurrence of this characteristic divot after 6 weeks of wearing the NTI during sleep alerts me that I'm highly likely dealing with a patient with 'Destructive' REM sleep bruxism. This topic has been covered in an earlier blog.
A well-controlled PSG investigation [5] had previously documented the high occurence of rhythmic masticatory muscle activity (RMMA) during REM sleep in patients with idiopathic REM sleep behavior disorder (iRBD). The latter is an extremely powerful predictor (or prodomal marker) of neurodegenerative synucleinopathies, including Parkinson disease, dementia with lewy bodies, and multiple system atrophy, and >80% eventually develop neurodegenerative disease[6]. Therefore iRBD should always be suspected and further neurologic assessment recommended to patients presenting with these divots after 6 weeks, especially when there is a family history of synucleinopathy. Only a laboratory-based level 1 sleep study can definitively differentiate sleep bruxism during REM or NREM sleep from other sleep disorders like oromandibular myoclonus/faciomandibular myoclonus, tooth tapping and sleep epilepsy.
It also dawned on me that the severity and characteristic pattern of wear observed on the discluding element of the NTI after 6 weeks usage together with a proper history and clinical examination could help us to better differentiate amongst the bruxism phenotypes. (Figs. 14-19) A patient can exhibit both NREM and REM SB (Fig. 14c) or any combination (Fig. 16).
In a discussion during the Faculty Seminar and PSG workshop, which was part of the Second Edmund Tay Mai Hiong Distinguished Speaker Programme (July 8-10, 2018), Prof. Gilles Lavigne suggested that we also look at the brief transition period from NREM to REM sleep as this was where he had found intense RMMA activity in some subjects. In any case, we hope these serendipitous findings will be independently verified or clarified by NUS researchers in a randomized controlled trial using full night attended level I PSG with concomitant audio-visual recording.
Fig. 14A & B REM SB wear on sleep NTIs
Fig. 14C Patient exhibiting both NREM & REM SB
Fig. 15
Fig. 16
Fig. 17 NREM Sleep Bruxism
Fig. 18 REM Sleep Bruxism
Fig. 19 Awake Bruxism
Protocol
For diagnostic considerations, I favor the NTI over other anterior bite stop systems (newer versions include Flexi Orthotic System, Bite Soft) mainly because of the consistent, published mechanical properties (including abrasion resistance) of the polycarbonate material (LEXAN Resin HP4) used in the manufacture of their relatively inexpensive blanks. Although chairside fabrication time can be significantly reduced if a thermoplastic material is used to fill the NTI blank instead of the more durable autopolymerizing acrylate, I strongly recommend you avoid the former. It would be almost impossible to predictably maintain patient’s gingival tissue health, ensure continued device retention and/or prevent untoward tooth movements over a 6 week period using a polycarbonate blank filled with porous, opaque, plaque-retaining thermoplastic material that cannot be properly polished. Primum Non Nocere!
Adjustments are always necessary and made along the outer surface (without perforating the polycarbonate surface) to ensure that at jaw closure and during excursive movements, resultant tooth contacts are present only between the device and the incisal edges of the antagonistic teeth. Bite opening should not be excessive although the minimum occlusal clearance between posterior teeth during all mandibular movements should be 1.5mm. The contact of the opposing incisors should be perpendicular to the surface of the discluding platform. The larger standard upper NTI device is used during sleep (remind the patient they need to use it if they nap during the day) whilst the lower device is used during waking hours as it interferes less with speech.
Note when the opposing incisor teeth edges are abnormally serrated or sharp they should preferably be smoothened down, i.e. with patient consent, as this might cause more or deeper scratches.
WARNING: Regular recall is essential as the NTI is a sectional occlusal coverage device and patients should be well informed that untoward tooth movements may occur if wear is not properly supervised. All patients sign an informed consent form to make sure they fully understand the diagnostic nature of this 6 week trial and are fully aware of all possible side-effects. If the device ever becomes unstable or can be removed easily with the tongue, they should immediately stop wearing it. They should also consult the dentist if when wearing the device, their posterior teeth can touch in any centric or eccentric jaw position. The patient must understand that gradual 'deprogramming' of postural muscles may allow the mandible to adopt a different upright postural rest position thereby altering the closing trajectory of the lower jaw. Thus most will likely notice a bite change when they first remove the device. This should be expected and patients should be careful, especially in the first few days when they remove the device to eat. Bite alterations tend to occur more frequently in patients who present originally without adequate anterior overbite. Pre-existing joint noises may also be unmasked. These are not necessarily indicative of pathology or ongoing disease but may reflect permanent morphofunctional adaptive changes that have occurred in the TM joint(s).
There will be those patients who will tell you that they absolutely cannot tolerate wearing the NTI for any period of time even though they themselves attest that the device was absolutely comfortable and passive when they first put it in. Others will fail to complete the 6-week trial and complain that the device prevents them from getting restful sleep despite numerous adjustments or re-dos. One should then suspect other underlying psycho-behavioral and neurologic factors like hypervigilance, anxiety, obsessive compulsive disorder, a low arousal threshold or even tactile/mechanical allodynia which is not uncommon in migraineurs.
NTI wear during sleep should be suspended after the 6-week diagnostic trial in those subjects who were found to exhibit REM SB. Previous biomechanical experiments have clearly demonstrated that maximum loading to the temporomandibular joints was sustained when subjects were biting on an anterior occlusal fulcrum[7]. Thus, without benefit of the protective Trigeminal jaw opening reflex during REM sleep, the TM joints will be vulnerable to damage. In other words, the NTI-tss and all anterior bite stop systems are contraindicated in patients exhibiting REM SB.
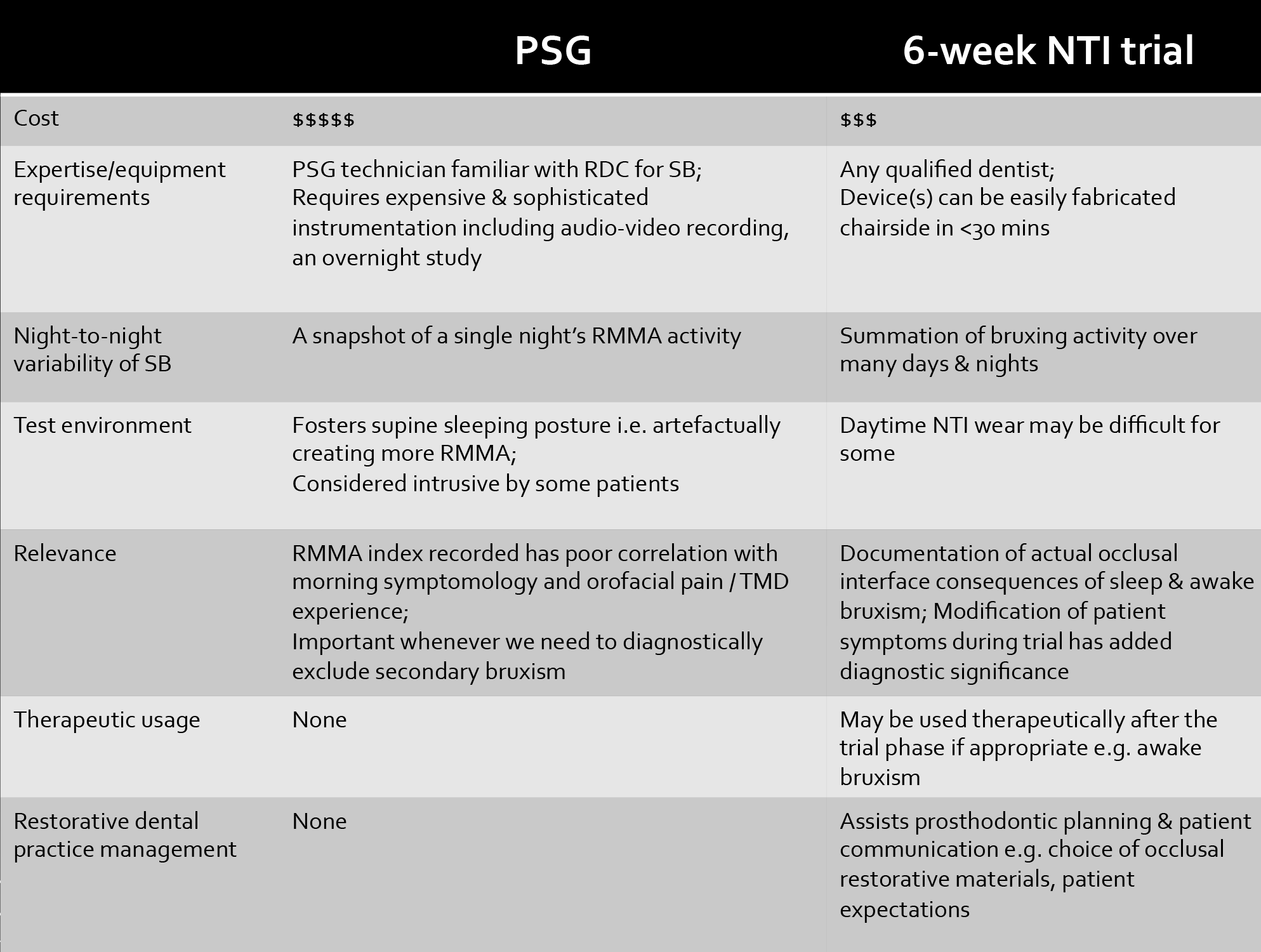
The comparison between PSG and the 6 week NTI trial is shown in Table 1.
Towards a phenotypic approach in bruxism management
The big advantage of this NTI trial is that it helps individualize patient treatment and allows dentists to make better judgements as regards their restorative plan. For instance, when patients actually see how much damage they could do to the sleep NTI in a matter of 6 weeks, it’s much easier to get them to be realistic about prognosis if they were at first unwilling to wear occlusal splints to bed. Even the most esthetic conscious may now consider metal on the occlusal surface in the restoration of their distalmost molars or at least assume greater responsibility for their decisions.
Many times patients are incorrectly prescribed full occlusal splints for sleep by their dentists when they only exhibited awake bruxism! The patient in Fig 12c) & 12d) had severe OSA (apnea-hyponea index of 88 events per hour) but exhibited no NREM or REM SB - only severe AB. He was very compliant and did extremely well on nasal CPAP therapy and continued using the awake NTI only during stressful periods and when planning or doing work on the computer.
The 34 year old patient in Fig. 4 was a very stressed ‘high flyer’ in the financial industry referred for the management of TMD/persistent orofacial muscle pain and migraine without aura. He was more concerned about the progressive wear of his dentition. His NTI trial showed he had NREM SB and AB. He also suffered from chronic fatigue, insomnia, excessive daytime sleepiness(Epworth Sleepiness Scale=14), nasal congestion (allergic rhinitis, deviated nasal septum, swollen nasal turbinates) and was a habitual mouth breather and a self-confessed OTC nasal decongestant 'junkie' who also used Ventolin almost daily. An overnight sleep study confirmed he had Upper Airway Resistance Syndrome(AHI=4, RDI=19) and very fragmented, unrestorative sleep. Besides cognitive behavioral therapy(CBT), we referred him for minimally invasive ENT surgery (radiofrequency inferior turbinate reduction and septoplasty) and addressed his sleep disordered with Appliance Therapy (i.e. he wore a mandibular advancement splint religiously during sleep). He successfully underwent a Buteyko /Oxygen Advantage programme to convert him into a nasal breather and continues to sleep with his mouth taped shut. He was also referred to a gastroenterologist who prescribed proton pump inhibitors for his concomitant GERD. His TMD condition, sleep and stamina improved so much that he didn’t feel he needed to do anything with his teeth, although he admitted that managing his work stress remained a challenge. For his parafunctional jaw clenching and associated masseter hypertrophy/headache, he preferred periodic Botox injections to wearing an NTI during the day. The frequency of his migraines has diminished significantly. This interesting clinical association between awake bruxism and migraine has been discussed in a previous blog.
Fig. 4
Fig. 17, 18 & 19 illustrates how the 6-week NTI trial can supplement a good history and physical examination in the identification of your patient’s unique phenotypic bruxism profile. Be mindful the latter may comprise a combination of the different bruxism phenotypes (i.e. Primary/Secondary/NREM SB/REM SB and/or Awake Bruxism).
Fig. 20 summarizes some of the behavioral, structural and medical/pharmacologic combination strategies that may be employed in the management of bruxers with complex comorbidities.
Fig. 20
Conclusions
There is an urgent need for a paradigm shift in how we approach the management of the bruxing patient. The proposed 6-week NTI trial can provide invaluable information to supplement a good history and physical examination in the identification of your patient’s unique phenotypic bruxism profile. One size does not fit all!
David K. L. Tay, BDS, MS
References
Stapelmann, H. and J.C. Türp, The NTI-tss device for the therapy of bruxism, temporomandibular disorders, and headache–Where do we stand? A qualitative systematic review of the literature. BMC Oral Health, 2008. 8(1): p. 22.
Becker, I., et al., Effect of a prefabricated anterior bite stop on electromyographic activity of masticatory muscles. Journal of Prosthetic Dentistry, 1999. 82(1): p. 22-26.
BAAD‐HANSEN, L., et al., Effect of a nociceptive trigeminal inhibitory splint on electromyographic activity in jaw closing muscles during sleep. Journal of oral rehabilitation, 2007. 34(2): p. 105-111.
Shankland, W.E., Migraine and tension-type headache reduction through pericranial muscular suppression: a preliminary report. CRANIO®, 2001. 19(4): p. 269-278.
Abe S, Gagnon J-F, Montplaisir J Y, Postuma RB, Rompre P, Huynh NT, Kato T, Kawano F, Lavigne GJ. Sleep bruxism and oromandibular myoclonus in rapid eye movement sleep behavior disorder: a preliminary report. Sleep Med, 2013. 10: p.1024-30.
Schenck CH, Boeve BF, Mahowald MW. Delayed emergence of a Parkinsonian disorder or dementia in 81% of older males initially diagnosed with idiopathic REM sleep behavior disorder (RBD): a 16-year update on a previously reported series. Sleep Med, 2013. 14: p.744-48.
Ito, T., et al., Loading on the temporomandibular joints with five occlusal conditions. Journal of Prosthetic Dentistry, 1986. 56(4): p. 478-484.
Note: Portions of the information on this blog on bruxism had been presented at the Singapore Sleep Conference 2017. Ref: Tay DKL: Bruxism Phenotypes – One size does not fit all! (26 August, 2017)
The views and opinions expressed in this article are those of the author's alone.